Certain varieties of pancreatic cancer exhibit multiple tumor cell subtypes that work, somewhat mysteriously, to quickly become resistant to chemotherapy agents. Researchers at Purdue University have now built a unique microfluidic device that can be used to test a cancer drug on multiple tumor cells subtypes. Using this technology the researchers believe that new drug therapies can be discovered and existing medicines used more effectively.
“The drug discovery and screening process has been using one cancer cell subtype and studying how it interacts with neighboring non-cancer cells, but this may overestimate the efficacy of the drug,” said Bumsoo Han, one of the Purdue leads on the research. “By condensing time to look at how cancer cells interact within a pancreatic tumor, we found that one cancer cell subtype can not only be more drug-resistant than the others, but drug-sensitive cells can also become resistant through interaction between the subtypes”.
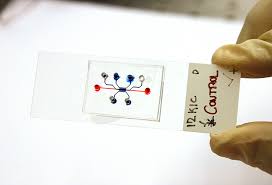
The new microfluidic device features specially designed collagen channels that function as the pancreatic duct on a very small scale. Within, a mix of cancer cells can grow and proliferate and various therapies can be delivered into the channels. In the past, similar devices have been used to work with late-stage tumor cells, but the new technology is intended to be used with earlier cell lines that have not yet mutated. This may help to find out which therapies are most effective at preventing mutations from happening.
“Not much research has been done on what kind of interaction happens within tumors, so those mechanisms of drug resistance have been overlooked,” added Han.
From the study abstract in Lab on a Chip:
We develop an in vitro microfluidic tumor model mimicking the heterogeneous accumulation of key driver mutations of human PDAC using cancer cells derived from genetically engineered mouse models. These murine pancreatic cancer cell lines have KPC (Kras and Trp53 mutations) and KIC genotypes (Kras mutation and Cdkn2a deletion). Also, the KIC genotypes have two distinct phenotypes – mesenchymal or epithelial. The tumor model mimics the ITH of human PDAC to study the effects of ITH on the gemcitabine response. The results show gemcitabine resistance induced by ITH. Remarkably, it shows that cancer cell–cell interactions induce the gemcitabine resistance potentially through epithelial–mesenchymal-transition. The tumor model can provide a useful test bed to study interaction mechanisms between heterogeneous cancer cell subpopulations.