Researchers at MIT have created a microparticle vaccine that can provide booster doses automatically. The hollow microparticles resemble a coffee cup with a lid, and are made using poly(lactic-co-glycolic acid), otherwise known as PLGA. The polymer breaks down over time in the body, releasing the contents of the hollow particles. By changing the composition of the polymer and the chemical groups attached to it, the researchers can tweak the release time, allowing them to deliver an assortment of particles that release at different times. This would allow them to deliver the particles subcutaneously, and then as the particles break down the recipient would receive their initial dose and then booster doses at later dates. The technology could help to provide long-term immunity without the need to attend a clinic on multiple occasions and could help with the logistics of large-scale vaccination campaigns, such as those initiated during the COVID-19 pandemic.
Vaccines are a cornerstone of public health initiatives, and have helped us to avoid the worst effects of many serious diseases and even eradicate certain diseases, such as smallpox. During the COVID19 pandemic, vaccines have provided some much-needed protection from the worst effects of the SARS-CoV-2 virus. However, the need to receive multiple doses of the vaccine, along with followup boosters, is a sticking point in terms of logistics. Missed appointments for second doses are always a possibility, and it would be easier (and likely cheaper) to just use a one-dose system.
This technology aims to achieve this, with booster doses becoming available within a vaccine recipient’s tissue over time. “This is a platform that can be broadly applicable to all types of vaccines, including recombinant protein-based vaccines, DNA-based vaccines, even RNA-based vaccines,” said Ana Jaklenec, one of the lead researchers that created the new technology. “Understanding the process of how the vaccines are released, which is what we described in this paper, has allowed us to work on formulations that address some of the instability that could be induced over time.”
To create the particles, the researchers use silicone molds to form the ‘cup’ shape out of the polymer mixture, and then ll the hollow structures with the vaccine. They then apply a polymer “lid”and heat the particles slightly to fuse the lid and cup together, sealing the vaccine inside. The researchers can tweak the release prole of the particles by using polymers with slightly different chemical properties. “If you want the particle to release after six months for a certain application, we use the corresponding polymer, or if we want it to release after two days, we use another polymer,” said Morteza Sarmadi, another researcher involved in the study. “A broad range of applications can benet from this observation.”
UK scientist create surgical ressing to facilitate and enhance photothermal therapy following melanoma resection
Scientists at the University of Nottingham in the UK have created a surgical dressing that is specically designed to facilitate and enhance photothermal therapy following melanoma resection. The dressing allows for nearinfrared photothermal therapy that lasts just 15 seconds every 48 hours. The concept involves killing any remaining melanoma cells, while encouraging healthy cells to regenerate within the resection site.
The dressing contains graphene oxide (a photothermal agent, which converts the energy from light to heat, killing cancer cells), elastin, and ethanol. Combining the graphene oxide with elastin reduces its cytotoxicity, meaning that it does not pose a threat to healthy cells, but still enables photothermal therapy to kill residual melanoma cells. The ethanol acts to help chemically reduce the graphene oxide, making photothermal therapy more efficient, and also forms an antiseptic component within the dressing.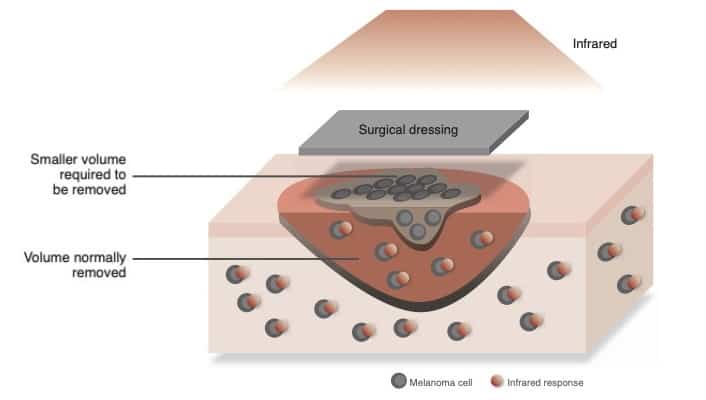
Melanoma is a highly aggressive cancer, and once detected, surgical resection is the most common option. However, surgeons frequently err on the side of caution and remove a large portion of tissue to ensure that they have excised all the cancer and help to prevent recurrence. Another option is to use photothermal therapy, where the resection site is exposed to light and a photo the rmal agent converts the energy from the light to heat , he lping to kill residual cells. If performed effectively, this approach could potentially allow surgeons to be more conservative in their resection.
“Given the aggressive nature of melanoma, surgical resections to remove it have to be signicantly larger than the size of the tumors to minimize the presence of residual cells,”said Yuanhao Wu, a researcher involved in the study. “This creates a new wound and delays healing. Beyond the prevention of tumor recurrence and promotion of tissue healing, our dressings could also lead to smaller surgical resections and practical post-surgery treatments that are non-invasive and could be delivered at home.”
It can be difficult to deliver photothermal agents to tumors through the bloodstream, as they can have an erratic blood supply and tortuous vasculature, and some photothermal agents can have negative effects on healthy cells. This latest technology aims to place the photothermal agent, in this case reduced graphene oxide, directly onto the resection site. So far, the researchers have shown that the dressings only require 15 seconds of irradiation with near-infrared light every 48 hours to produce effective photothermal therapy. Patients could even administer the light therapy by themselves at home.