Described as a diagnostic imaging technique primarily used to visualize viscera & other internal structures in the body, ultrasonography utilizes the properties of sound
Ultrasonography (US) is an integral modality in healthcare in general but even more so in emergency care. This technology has become a pivotal part of the care that is administered to patients who are admitted for emergency care. Over the past few decades there has been an exponential increase in the use of ultrasonography which has become the standard of care for an emergency patient. Unfortunately, the awareness of this modality is not as  pronounced in healthcare culture as it should be and therefore this article will seek to shed some light on the importance of ultrasound in acute medicine.
pronounced in healthcare culture as it should be and therefore this article will seek to shed some light on the importance of ultrasound in acute medicine.
Ultrasonography is a diagnostic imaging technique that is primarily used to visualize viscera and other internal structures in the body. It works based on the principles of physics by utilizing the properties of sound. Sound waves with frequencies greater than those audible to the human ear, appropriately named ultrasonic waves, are sent as pulses through a transducer into the body which are then reflected back as echoes of varying degrees depending on the physical properties of the tissue they reflect off of.
These echoes are then recorded and displayed as an image which is used by the operator to further his clinical impression or strategy. The primary advantages that make ultrasound superior to other imaging modalities is its ability to provide the healthcare professional images in real-time without the use of ionising radiation which is a considerable disadvantage encountered with other imaging modalities.
Invaluable utility in healthcare
Ultrasound applications offer advanced diagnostic and therapeutic tools to facilitate patient care with minimal requirements in capital, space, energy or training hence making it an invaluable utility in acute medical care. It is also the most cost effective imaging modality available for recurrent use. Ultrasonography is a science that is taught at every standard of medical education in one form or another displaying the importance of understanding the dynamics of ultrasonography and the value it adds to a healthcare professional upon acquiring the skill of operating the probe and interpreting the sonograms.
Ultrasound imaging and information systems are increasing in integration and sophistication providing more  versatility and mobility in use of the modality. The hardware and equipment required to use ultrasound is diminishing in size as we progress into the future with instruments now available the size of the smartphone with the added benefit of wireless connectivity which integrates the device to the Electronic Medical Records (EMR) and Picture Archive Communications System (PACS). The practice of using ultrasound in medical practice is growing and has found its place in the world of emergency medicine.
versatility and mobility in use of the modality. The hardware and equipment required to use ultrasound is diminishing in size as we progress into the future with instruments now available the size of the smartphone with the added benefit of wireless connectivity which integrates the device to the Electronic Medical Records (EMR) and Picture Archive Communications System (PACS). The practice of using ultrasound in medical practice is growing and has found its place in the world of emergency medicine.
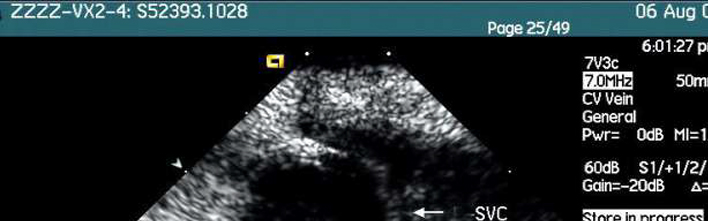
Emergency Ultrasound (EUS) is used to evaluate acute and critical medical conditions and it is utilized for numerous medical reasons like diagnosis, resuscitation of the acutely ill or injured patients, guidance of medical interventional procedures, monitoring of specific pathological conditions and as an adjunct to therapy. EUS examinations are performed and interpreted by emergency physicians in both, in-hospital and out-hospital settings. EUS is interchangeably also used instead of terms like point of care or focused ultrasound. EUS is a distinct entity from physical examination that provides the physician with anatomical & physiological data that is otherwise not acquired through methods used in a physical examination like inspection, palpation or auscultation.
EUS is classified into the following functional clinical categories:
• Resuscitative
• Diagnostic
• Sign and symptom based
• Procedural guidance
• Therapeutic and monitoring
There are 12 functional US applications where it is applicable to use the modality efficiently:
• Trauma
• Pregnancy
• Cardiac and Hemodynamic assessment
• Abdominal aorta
• Airway
• Biliary
• Urinary tract
• Deep venous thrombosis
• Soft tissue and musculoskeletal
• Ocular
• Bowel
• Procedural
ER physicians are therefore trained and educated in basic ultrasound physics, instrumentation, procedural guidance and Focused Assessment with Sonography in Trauma (FAST). This leads to ultrasound guided procedures which provide safety in performing a wide variety of procedures involving drainage, US guided nerve block and vascular access which without the existence of US would expose the patient to great risk. Overall these methods not only increase the standards in patient safety but also allow the treatment of pain in patients without the side effects encountered with systemic opiate use.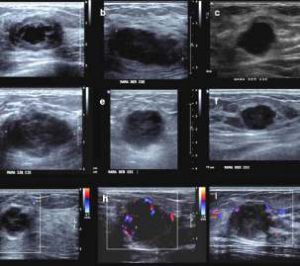
The existence of EUS in our healthcare system is greatly advantageous but it also serves as an invaluable tool in other subsets of the population for different reasons. The paediatric population of patients benefits greatly from this as they are at a greater risk when it comes to ionising radiation exposure hence US serves as the most appropriate imaging modality. Furthermore, US is used widely in critical care, prehospital settings and in rural and remote areas where access to technology is limited. Its use is also of paramount importance in disaster medicine and when addressing global public health issues.
Evolving spectrum
Training is provided to healthcare professionals and is based on a wide array of principles which are in line with the evolving spectrum of training in clinical ultrasonography. They are introduced to the skills required in operating the device and applications are taught along with core concepts that are reinforced. In line with the evolution of both medical education and the advancement of the technology embedded in US devices innovative educational strategies are implemented to provide environments for learning that prepare the practitioner for using the skills acquired in a clinical setting. This is done through problem based scenarios and simulated cases upon which the practitioners practice before implementing their learned skills in the clinical settings whether they be in-hospital or out-of-hospital.
As previously mentioned, the advantages of this imaging modality are immense and improving. Patient safety is the headline, however it also decreases medical mistakes during procedures leading to more patient satisfaction. There is an improved utilization of the departmental resources, eliminating invasive procedures which are not cost friendly. Overall, utilization of the US modality leads to improved clinical decision making and therefore a better outcome in patient care.
The future of EUS has already been given birth to as wireless transducers and handheld systems are readily available at many healthcare institutions. This will not only allow an expanded availability of US to clinical settings at affordable rates. Telesonography is another innovation that allows for graphical data to be transmitted from remote locations to centers that can offer consultations and treatment strategies over a distance. An increased number of multi-centre studies will allow the emergence of higher levels of evidence which would lead to the development of more guidelines that can better direct acute medical care whilst simultaneously promoting the use of US in medicine.